Planet of the Strains
Why there are new variants of COVID cropping up and this pandemic isn’t ending anytime soon.
Why there are new variants of COVID cropping up and this pandemic isn’t ending anytime soon.
By anyone’s standards, 2020 was…not fun.
(Remember when we thought the fires in Australia would define the year to come? Yeah. Me neither.)
But after all that doom and gloom, it looks finally as if there may be a light at the end of the tunnel: vaccines.
All over the world, vaccine administration has been rolled out in the past few months. The USA has distributed over a hundred million doses, India almost fifty, and the Seychelles a grand total of one hundred thousand — although that’s actually around 60% of their population.
Going into April, most countries are beginning to move forward from those most critically at risk to distribute vaccines on a wider scale. But with the threat of new strains and so many different vaccines being offered, it’s easy to feel overwhelmed.
Allow me to remedy that.
It begins when you inhale.
The mucus and hair in your nostrils traps dust, pollen, and pathogenic particles that might otherwise irritate or scratch up the sensitive tissue lining deeper in your nasal passages — like the coronavirus.
Your immune system is made up of two parts that work together to prevent bacteria and viruses from damaging your body. The first is your generalized/general response.
Some particles, like COVID-19, are too small to be caught in this trap. They pass into your body and enter the lungs, where they can proliferate and enter the bloodstream. But as soon as these pathogenic particles get into your bloodstream, white blood cells (WBCs) called neutrophils and macrophages try to break them down before they can cause real damage.
In the case of viruses, the WBCs try to engulf the pathogen, surrounding it and releasing enzymes that can destroy its proteins and genetic material. It’s neutralized before it can hijack your body’s cells to reproduce and make more virus particles.
But if these defenses fail, the virus can enter your cells and take over your personal protein making mechanism. It can then forcibly create more viruses that travel through your body and cause dangerous symptoms like the respiratory failure and heart problems we see in some people with COVID-19.
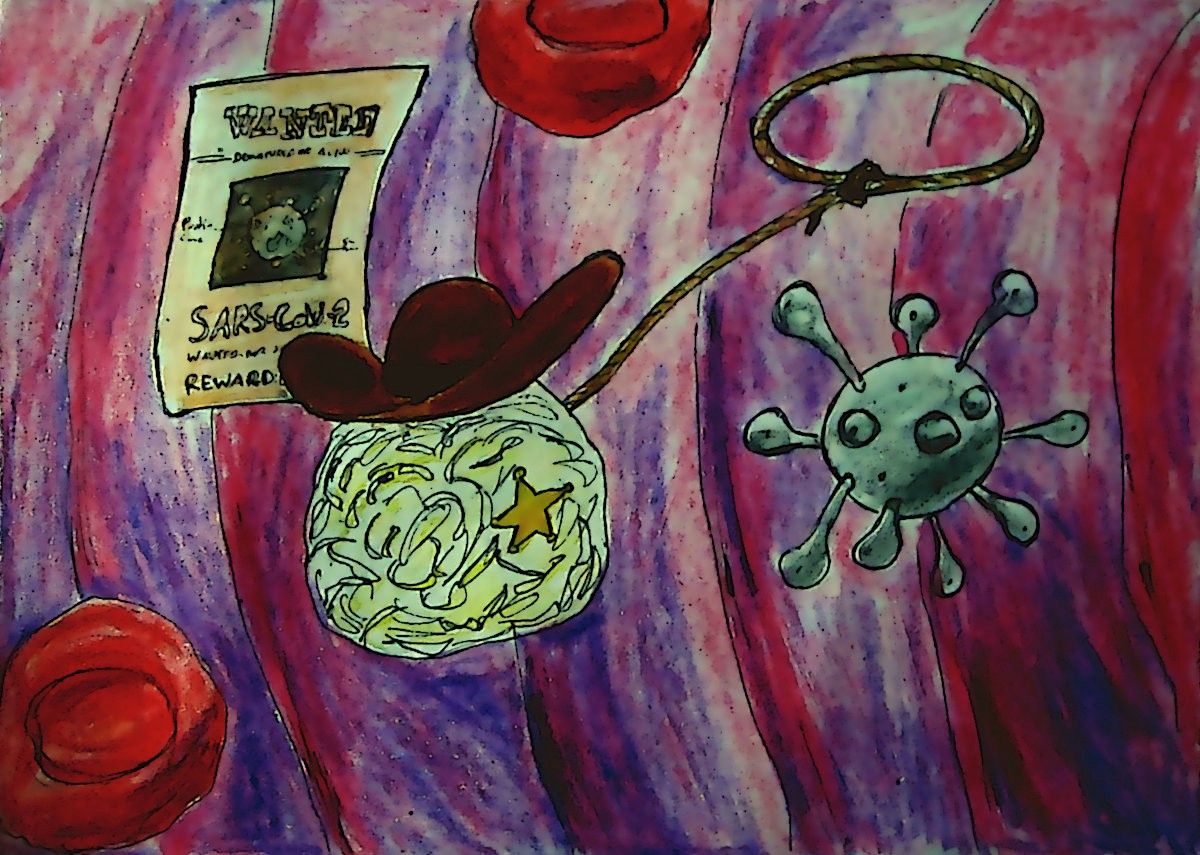
Think of a sheriff in those old Westerns who walks into a saloon at high noon. Everyone and everything that looks like it doesn’t belong is under suspicion and going to be questioned. Similarly, WBCs will process any particle they think doesn’t belong in the body. These generalized defenses don’t discriminate. They attack all potential threats the same way. In fact, they are so indiscriminate that they sometimes attack peanut, milk, shellfish or pollen particles (i.e. allergic reactions).
Of course, no Western sheriff truly goes about arresting people willy-nilly. He has wanted posters to tell him what sort of bad guy to look out for.
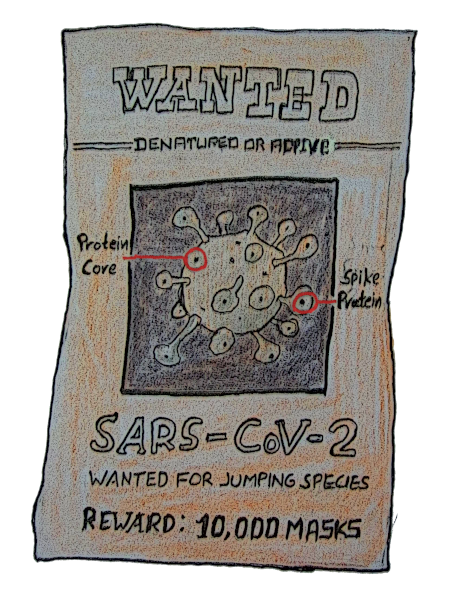
The body has its own sort of wanted posters. The first time you’re infected with a bacteria or virus, the macrophages we talked about earlier surround the pathogen and identify its specific surface proteins. Called antigens, these proteins appear in specific combinations on each virus. Your body’s B-cells will then produce antibodies that specifically bind to those antigens and recruit other cells to come destroy the pathogen.
These antibodies then stay in your immune system’s memory, which maintains a rough sketch of the antigens of specific pathogens, and keeps your cells on high alert for any intruders or invaders with similar surface proteins. These intruders can then be attacked faster and with more strength if they try to show their ugly mugs around the body again. Sometimes, though, this response still might not be enough to destroy the virus when it comes back, which is how reinfection happens.
Traditional vaccines work by injecting you with just those surface proteins, or a denatured version of the pathogen. Denaturation is when the harmful parts of the pathogen are destroyed through heating or chemical treatment, while those surface proteins are left intact. This way, your body will be able to mobilize the antibody defense without being hurt by the virus itself.
When it comes to COVID-19, these surface antigens are called “spike proteins” and are generally harmless. It is the genetic material and enzymes inside the virus (the ones destroyed by denaturation), that cause the complications usually associated with COVID-19.
But mRNA vaccines take it a step further. Or back, if you want to get really technical!
All proteins in the world can be coded for in DNA, which acts as a template to produce mRNA. And mRNA, in turn, then acts as a template to produce the actual surface proteins.
So rather than injecting you with the spike proteins or denatured COVID-19, mRNA vaccines inject you with the mRNA needed to make spike proteins in your own cells, which then start up the immune response. Since mRNA is naturally broken down in your body after use, this vaccine is not that different from traditional vaccines in terms of endgame.
DNA vaccines are where things get trickier.
Before I rile up any anti-vaxxers or conspiracy theorists, I would like to say that similar treatments have been heavily studied in animal models. These vaccines are extensively tested. This technology has been researched heavily in recent years, even before the pandemic.
This isn’t Rampage; you don’t have to worry about turning into a titanic rage-beast.
DNA vaccines go to the real basics, by splicing the DNA needed to make spike proteins into your own genome. As with mRNA vaccines, your body then makes the spike proteins by itself, prepping your immune system to guard against future infections. But because it is altering your DNA itself, this type of vaccine thus has more long-term ramifications than mRNA and traditional vaccines.
Similar technology has also been used to cure sickle cell diseases in living human subjects and has great therapeutic potential. Sickle cell disease is caused by a point mutation, which occurs when one out of the billions of bases in your DNA is wrong. Specifically, it occurs when glutamic acid replaces valine. By injecting patients with a vector of DNA that isn’t mutated, medical researchers were able to reverse the effects of the mutated DNA and cure sickle-cell related ailments.
Now, you’ve probably heard of genetic mutation through science fiction movies or high school biology. Think Marc Webb’s The Amazing Spider-Man or Steven Spielberg’s Jurassic Park.
Remember how genes determine protein structures? Similarly, mutations in a virus can thus lead to changes in the structure of its spike proteins, as well as its infectiousness. And if the spike protein’s shape changes, the antibodies in your immune system memory won’t recognize them properly.
It’s like if the wanted criminal rolled up to the saloon with a disguise on: some people might recognize him vaguely, others might not at all. Similarly, vaccines based on spike proteins from one strain might be limited or totally ineffective in arming your immune system against infection and illness from these new strains of COVID-19.
That’s why everyone is suddenly in a tizzy about the different strains of COVID-19. If our body can’t recognise the infection, how are we supposed to beat it?
So: which vaccines do what? Which ones are the most effective, most protective, and most accessible? Well, like so much else of what we’ve talked about, the answers to those questions aren’t very easily defined.
Just as new strains are emerging around the world nearly every week, scientists are discovering new data too. Some researchers are testing whether the vaccines reduce symptoms, others whether they reduce reinfection rates, and still others at how effective the vaccines are for multiple variants. And a good deal of this data tends to vary based on geographic location as well.
All vaccines measure efficacy as the rate at which it reduces symptomatic COVID-19 cases, typically in people over the age of 18. In double-dose vaccines, this measure is taken after the second dose - obviously, a single dose wouldn’t be nearly as effective. All vaccines do have some side effects in certain patients, ranging from hypersensitivity to anaphylaxis, but none of the ones that we’ll discuss have displayed any to an alarming extent.
The first is the Janssen vaccine - the only traditional, single-shot vaccine - which currently seems to have a 72% efficacy - but that number does reduce to 66.3% in Brazil, and 64% in South Africa.
After both doses, Pfizer-Biontech’s vaccine has a 95% efficacy, even when accounting for gender and ethnicity, and even for high-risk populations such as those with diabetes or asthma. The company has released some data that suggests that the vaccine is effective against the new strains emerging in the UK and in South Africa, although less so than for the non-mutant strain. It’s important to note, though, that this information comes only from genetic models and not actual samples of the virus - but more studies are in the works.
The Moderna vaccine has a 94.1% efficacy rate, although it drops to 90.9% for high-risk patients, such as those with diabetes and prior HIV infections, chronic lung, liver and/or heart disease. The levels of specific antibodies against the South African and UK strains were much lower than they were for the non-mutant strain of COVID-19, but researchers believe they’re high enough to offer protection from the worst symptoms.
Both the Moderna and Pfizer-Biontech’s vaccines offer around 50% efficacy after only one dose, typically kicking in over two to three weeks. You need to get both doses for the full effect.
In exciting news, both Moderna and Pfizer-Biontech’s vaccines also show some promise for treating pregnant women. Scientists are also theorizing that mothers who get vaccinated could pass on the antibodies to their children through the umbilical cord blood and breastmilk..
Lastly, the Astrazeneca vaccine has a 59.5% efficacy in reducing the same thing as the other three, although a recent press release has suggested that the number might be as high as 76%. It was recently withdrawn from use against the South Africa variant due to ineffective preliminary results.
At the time this is published, the EU has authorised all four while the United States continues to hold out on Astrazeneca because of some issues with data and transparency. Interestingly, India has authorised the Astrazeneca vaccine, as well as its domestically-produced COVAXIN which is produced by Bharat Biotech and appears to have an efficacy of around 80%.
There are some questions about how much the time of research has affected efficacy rates, though. Pfizer-Biontech and Moderna began testing in 2020, when COVID-19 hadn’t had much time to mutate. Since nearly everyone was infected with the same strain, the vaccines showed high efficacy in reducing COVID-19 symptoms. However, the new Janssen (i.e. Johnson and Johnson’s) vaccine began testing later, once mutant strains started becoming more prevalent, which might have affected the data as well.
It’s likely that most of us will be vaccinated in 2021. It’s likely that the world will begin to move again, thawed out of the limbo it’s been in for over a year. It’s likely, but it isn’t a guarantee.
Vaccines only protect the person who’s been vaccinated, so vaccinated people can still be contagious. There is still a risk that you could be reinfected, or infected by a different strain.
This pandemic continues to rage, and probably will for some time to come. It’s important to remember that it will only end when we bring an end to it. Part of that involves vaccines, yes, but it also involves continuing to do what we’ve been doing all along - wearing masks and socially distancing.
So stay well, stay informed, and - as so many of us have begun signing off our emails lately - stay safe.
Stay informed: The World Health Organisation’s COVID Dashboard.
Hold it in your hands: Would you like a printed magazine of 80+ pages packed with more great writing like this? The Snipette membership programme allows you to do just that — and helps fund thepublication too. Click here to start supporting us.
