Force of Habit
Neural firing and wiring in our most stubborn behaviours
Neural firing and wiring in our most stubborn behaviours
If you’ve ever had a pet, you’ve probably seen how eager they are around mealtime or even when they hear the sound of a can opener. While it might be harder to picture pigeons in the park dancing for scraps of bread from passersby, a few simple experiments throughout history have shown us how easy it is for anyone to succumb to conditioning.
This concept was elegantly demonstrated in dogs in the early 1900s — by the Russian psychologist Ivan Pavlov — and came to be one of the most famous examples of its kind in psychology. The basic idea is that our brains can form associations between previously unrelated events to guide our behaviour in unexpected ways.
Pavlov’s dogs, for example, grew so accustomed to hearing the sound of a bell ring when food was presented that, eventually, all it took was the sound of the bell to make them salivate. Though many of us may have learned about some version of this experiment in school or the media, fewer of us might recall Skinner’s Pigeons.
While it may not have the same ring to it, the behavioural psychologist B.F. Skinner elegantly demonstrated the tendency of conscious organisms to become creatures of habit — even if those habits are somewhat bizarre. The experiment he conducted was simple: a hungry pigeon was placed in a box with a food dispenser that would produce pellets on a regular schedule.
Hunger was a crucial element of the experiment, as it meant the pigeons would find their food more rewarding when it arrived and they’d be more likely to learn if they knew there was a reward in it for them. Outside of any experimental training, though, the experimenters began to notice something odd.
Each of the birds being tested sometimes fidgeted or moved around anxiously over the course of the experiment, but right around mealtime, they would perform specific behaviours that they hadn’t been trained to perform. Some would walk in a counter-clockwise circle for a specific period of time right before the pellet drop. Others might hop in place a certain number of times.
It seemed that whatever the pigeons happened to be doing at the time of their first food reward became a ritual they performed, as though it brought about the delivery of their treats.
Inadvertently, Skinner had created “superstitious” pigeons.
No real association existed between the hops and fidgets the birds performed and the timing of their meal delivery, but because an association formed in the birds’ brains, they continued to go through the motions they presumably believed would bring about relief from their hunger.
To me, this experiment is less interesting as an example of conditioning than it is as a testament to the fundamental need we all have, to know that our environments are predictable and that we are capable of controlling them.
Our brains cope with unpredictability in a wide variety of ways. Some of us may experience deep anxiety and unwanted thoughts, that seem to play on endless loops in our heads.
When these behaviour patterns become severe and consistent, they may lead to a diagnosis of obsessive-compulsive disorder. While OCD has been reported to be just as debilitating and life-altering as other serious neuropsychiatric or neurological illnesses — like schizophrenia or Parkinson’s disease — patients who live with OCD frequently recognize that their obsessions don’t necessarily make sense. This may intensify their distress and make it difficult to reach a diagnosis if they’re reluctant to share the extent of their symptoms with their therapists.
The obsessive part of the disorder might come in the form of thoughts that can’t be chased away: intense mental revisiting of events that might not necessarily be significant, or distressing mental images that persistently reappear in the mind's eye.
Compulsions follow as a response to the anxiety that builds around obsessions; behaviours become tied to thoughts as the patient attempts to keep unwanted thoughts in check.
Many psychiatrists have found that people who develop obsessive-compulsive disorder (OCD) tend to crave a sense of control over their lives, and may develop compulsive behaviours or rigid sets of routines in an attempt to restore inner order.
Sometimes, these intrusive thoughts seem to come out of nowhere. They might also centre around everyday anxieties or worries and gradually rise to an unmanageable pitch.
This was the case for Karen Rusa, who after a period of depression and anxiety, began to fear that horrible calamities had befallen her children. Eventually, she adopted elaborate rituals that she believed she had to perform to keep them safe. If she failed to complete any of these rituals, she held herself personally responsible for the inevitable scrapes, bruises, or minor accidents that occur regularly in a household of four young children.
Rusa had grown up in a strict religious household, had married young, and was quickly overwhelmed with a large family of her own, shouldering most of the responsibilities of childcare and running the household on her own.
Lack of control — it seemed to her doctors — was a theme in her life. They attributed some of her distressing thoughts, and the behaviours she relied on to cope with them, to the chaos she lived with daily. Her compulsions also seemed to echo some of the strict rituals and observances prescribed by the church as she was growing up.
While personal history and life circumstances play heavily into a psychiatric diagnosis, the interaction between these factors and a patient’s basic neurochemistry always needs to be considered as well.
Neuroimaging studies have hinted at overactivity in several parts of the brain in OCD patients. In particular, pathways and circuits involved in learning associations between cues and rewards, and those that govern planning of complex actions and emotional regulation, seem to be more active in these individuals.
An eternal challenge in the treatment of complicated neuropsychiatric illnesses is that these pathways may be inherently overactive, leading to the symptoms of the illnesses. Or, they may be modified and reinforced by the behaviours themselves, upending cause and effect when it comes to diagnosis.
It can be difficult to target widely distributed activity patterns with conventional psychotropic medications, so other kinds of therapies — that seem to operate by addressing neurological functions at a higher level — have garnered intense interest in the neuroscience and psychiatric fields.
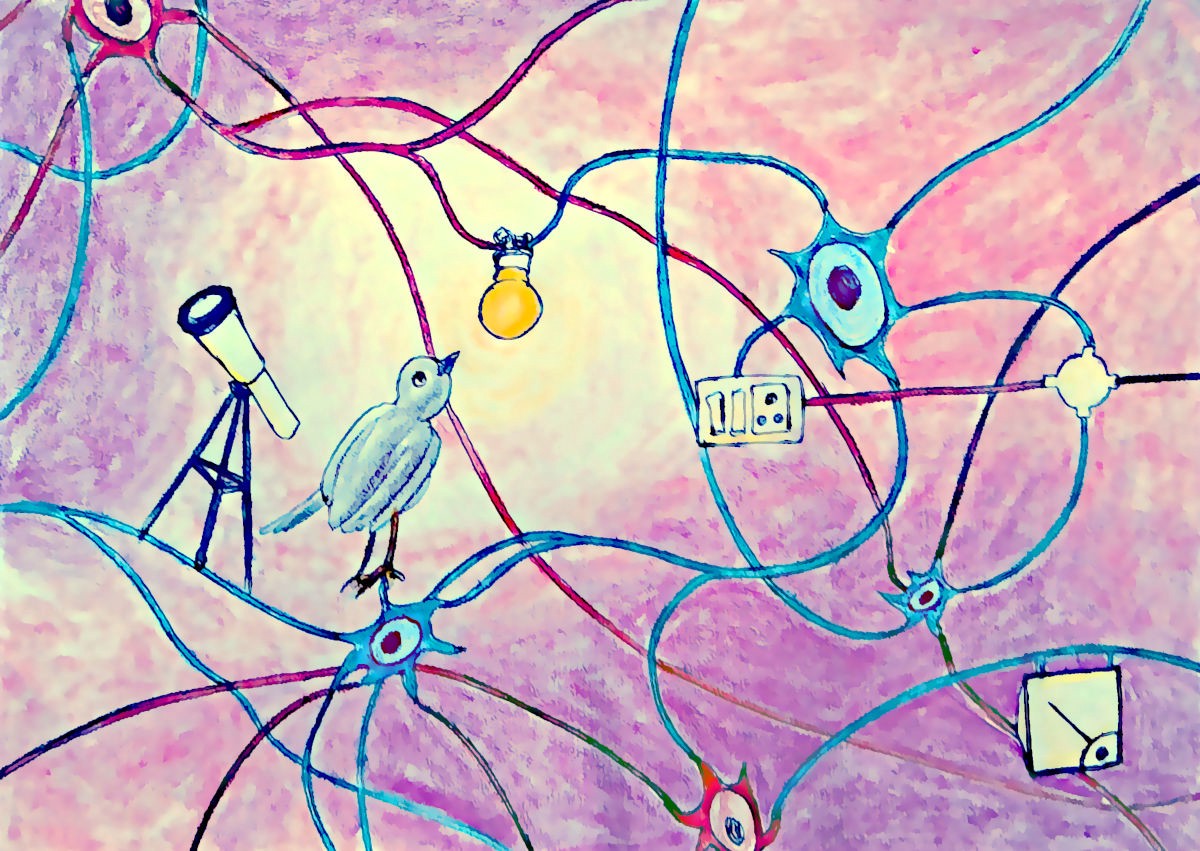
You can think of it a bit like remodelling an old house: while traditional antidepressants might be akin to changing a burned-out lightbulb here or there, these new classes of therapies are more like electricians — overhauling the faulty wiring.
An alternative to traditional drug therapy that seems to hold promise for obsessive-compulsive disorder and severe depression is transcranial magnetic stimulation. Abbreviated as TMS, it takes advantage of electrical pulses delivered by a magnetic coil through the scalp — clinicians can target activity to parts of the brain that are thought to be responsible for the distressing behavioural symptoms of these illnesses.
Pharmaceutical therapies act chemically on neurotransmitters and the receptors they bind with. But the problem is that these chemical messengers serve many different functions, and they’re found in multiple types of cells throughout the brain. They can have a variety of unpredictable side effects because they do so many things, some of which are still unknown.
An especially serious risk of many common antipsychotic medications is tardive dyskinesia — a phenomenon that mimics Parkinson’s disease and may come about after long-term use of these drugs. Because the neurotransmitter dopamine affects both mood and movement, it’s difficult to disentangle the short-term benefits for the former, and the long-term effects on the latter.
On the opposite side of this coin, Parkinson’s drugs that target dopamine to restore motor function have also been reported to cause mood and impulse control changes.
Antipsychotic and antianxiety drugs can also cause serious metabolic complications, leading to significant weight gain and enduring changes in the body’s ability to regulate blood sugar. The cellular mechanisms responsible for these kinds of side effects haven’t been extensively studied, so clinicians remain largely in the dark about how to prevent them. This broadens the appeal of alternative treatment strategies that run far fewer of these risks — collectively termed “off-target” effects.
The principle behind TMS is to change electrical activity directly, at a local level within the brain. It’s often said that cells that “fire together wire together,” referring to what neuroscientists call plasticity. This is the idea that the more certain pathways or sets of cells are activated — by a thought, behaviour, or experience — the stronger the connections between them become.
This basic principle allows us to learn new behaviours or flexibly adapt old ones to new situations. Behavioural circuits might be adjusted in this way, but they can also be retrained after repeated bouts of the same kinds of new and different activities.
Other unconventional therapies have succeeded where pharmaceuticals have failed, and they seem to operate by the same logic.
One recent study in a mouse model of depression revealed that low doses of psilocybin relieved some of the symptoms the researchers observed in animals similar to human readouts of depression. A low dose of ketamine can also be a highly effective antidote to stubborn depressive symptoms, and the effects appear to be longer lasting than traditional treatments.
Perhaps the most remarkable feature of ketamine is the speed with which it operates, at least in depression. While patients are usually advised that it may take several weeks of treatment with mainstream antidepressants for them to start to feel a difference in their moods, a single ketamine infusion works immediately — on a scale of hours, not weeks or months.
Neuroscientists have speculated that this rapid mood lift might come from the ability of ketamine to activate cellular pathways that stimulate synapse growth and the production of proteins, which help nerve cells form new connections to each other, enhancing the brain’s plasticity.
Like TMS approaches, the secret seems to lie in the ability of these compounds to coax the brain into shifting and adapting its own activity patterns and forming new connections between nerve cells.
One study on a specific kind of treatment-resistant depression — that often follows a stroke — found that applying TMS to specific parts of the brain that were involved in complex decision making and emotion, could initiate the same kinds of processes that happen when we first learn new information. It could also initiate the processes that occur to reinforce those new connections.
Both involve the generation of new proteins: electrical and chemical bridges between nerve cells that are re-engaged when we remember the information we’ve already learned.
The difference is subtle, but similar to a skilled electrician or carpenter; these kinds of therapies can help the brain build a scaffold that will stand the test of time.
The chemicals they seem to operate most heavily on act as neurotransmitters. But, they do so broadly to promote growth and activity, rather than the highly specific chemicals that work well to patch a leak here or some peeled paint there, but ultimately don’t tackle the problem at its core.
The beauty of the human brain, though, is that our wiring isn’t fixed. With a nudge in the right direction, our brains can begin to learn how to rewire themselves.
